Our RCM Services Elevate Your Practice to New Heights of Accomplishments While Keeping You Ahead of Customer Expectations.
Enhance your healthcare practice with our tailored and seamless Physician Credentialing Services. Our skilled credentialing specialists streamline the enrollment process, helping you save time and resources while maximizing your revenue opportunities.
Our Results-Oriented Revenue Cycle Management Services Ensure Fast Reimbursements.
Leverage Best-in-Class Revenue Cycle Management Services to Reduce Account Receivable Days by 25%, Improve Financial Health, and Achieve Operational Excellence.
Discover Our Advanced Revenue Cycle Management Services to Reach Your Financial Goals.
We Provide Free Trial Healthcare Revenue Cycle Management Services Before You Commit to a Month-to-Month Contract.
0{{current_slide_index}} | 0{{total_slide_count}}
Why are Healthcare Revenue Cycle Management Services Important?
Are you struggling to manage your Revenue Cycle Management effectively? Finding it hard to maintain smooth operations while hitting revenue goals? If these financial and administrative tasks are taking too much time and distracting from patient care, outsourcing to a trusted RCM provider could be your solution.
AM Billing Care brings years of experience working with healthcare organizations across the U.S. We offer affordable RCM services that can save you up to 60% on costs while ensuring HIPAA compliance and data security. Our team specializes in maximizing revenue by recovering underpaid claims, handling insurance follow-ups, and managing all aspects of the revenue cycle – from eligibility checks to proper coding.
By partnering with AM Billing Care, you’ll see improved payment collections, higher revenue, and more time to focus on your patients.
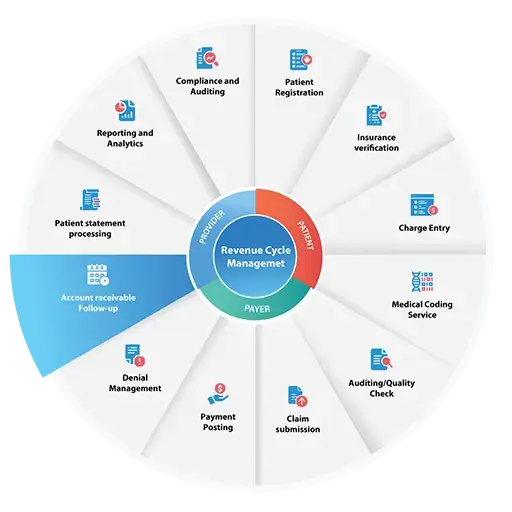
Patient registration is a crucial first step in healthcare revenue cycle management. It involves collecting complete patient details and verifying insurance coverage before appointments occur. Handling this properly helps medical practices create a solid foundation for smoother billing processes. Getting registration right from the start reduces paperwork, helps avoid claim denials, and gives patients a better experience from their first contact with your practice.
Insurance verification is a critical component of revenue cycle management that confirms a patient’s coverage and benefits to ensure accurate billing and reimbursement for healthcare services. Proper verification reduces claim denials, accelerates payments, and clarifies patient financial responsibilities. AM Billing Care’s thorough verification process promotes financial transparency and supports efficient revenue cycle operations. A robust verification system is essential for maintaining clear billing processes and delivering cost-effective care.
Charge entry is a crucial step in Revenue Cycle Management where healthcare providers document all procedures, services, and supplies provided to patients. Accurate charge entry ensures proper billing and reimbursement while maintaining compliance with regulations. This process plays a vital role in maintaining financial transparency and stability for healthcare organizations. AM Billing Care’s precise charge entry procedures help ensure correct claims submission and optimal revenue capture.
Medical coding assigns standardized alphanumeric codes to medical diagnoses, procedures, and services. Coders review patient medical records – including doctor’s notes, lab results, and treatments – to apply the correct procedure and diagnosis codes required for insurance claims. Proper coding is essential for accurate billing and revenue cycle management.
AM Billing Care’s coding team consists of AAPC and AHIMA certified professionals, including Certified Professional Coders (CPC) and Certified Coding Specialists (CCS). We perform all coding according to clinical documentation and client-specific protocols. Our specialists also review coding-related claim denials, make required corrections, and resubmit claims to enhance reimbursement rates and optimize revenue cycle performance.
AM Billing Care maintains rigorous quality control through continuous audits and checks. Our skilled team focuses on enhancing your revenue cycle management by ensuring accurate and timely claim submissions. With extensive training and experience, we consistently deliver high-quality results to optimize your financial performance.
Claim submission plays a critical role in Healthcare Revenue Cycle Management, requiring providers to compile and submit claims to insurance payers for reimbursement. Accuracy is essential, as errors can result in claim denials and delayed payments.
Effective claim submission depends on proper coding, adherence to payer guidelines, and complete documentation. Streamlining this process is key to securing timely reimbursements and maintaining the financial health of healthcare facilities. AM Billing Care’s expertise ensures claims are submitted correctly and efficiently.
Payment posting is a critical step in the revenue cycle where payments from patients, insurers, and third-party payers are recorded and applied to patient accounts. This process requires accuracy to properly track payments, outstanding balances, and patient responsibilities.
Effective payment posting is essential for medical revenue cycle management as it minimizes errors, facilitates financial reconciliation, and supports accurate reporting. This function plays a key role in maintaining reliable financial records while enhancing overall revenue cycle efficiency. AM Billing Care’s systematic approach ensures payments are posted correctly and efficiently.
Denial management plays a crucial role in healthcare revenue cycle management by identifying, analyzing, and resolving denied insurance claims. Unaddressed claim denials can result in significant revenue loss for healthcare providers. This process involves examining denial reasons, correcting errors, and resubmitting claims to obtain proper reimbursement.
An effective denial management system does more than recover lost revenue – it provides valuable data to improve future claims processing and prevent recurring denials. AM Billing Care’s denial management services help healthcare facilities minimize revenue leakage while gaining actionable insights to strengthen their revenue cycle performance.
Accounts receivable follow-up is an essential component of revenue cycle management that involves tracking and collecting unpaid balances from patients, insurers, and third-party payers. Effective follow-up procedures help healthcare organizations reduce outstanding receivables, accelerate cash flow, and minimize bad debt. This process requires persistent communication with payers and patients to resolve unpaid claims and balances, ultimately improving financial clarity for providers. AM Billing Care’s systematic approach ensures timely resolution of outstanding accounts while maintaining compliance and patient satisfaction.
Patient statement processing is a key component of revenue cycle management that handles the generation and delivery of financial statements to patients. These documents outline provided medical services, associated charges, and the patient’s remaining financial responsibility after insurance payments.
This process enhances transparency and patient engagement by clearly communicating healthcare costs. For providers, it delivers accurate financial information that fosters patient trust while improving payment collection efficiency. AM Billing Care’s statement processing helps healthcare organizations maintain financial stability through clear patient communication and streamlined billing procedures.
Revenue analysis and reporting serve as foundational elements of revenue cycle management. This phase involves evaluating financial data to thoroughly assess a healthcare facility’s fiscal performance and operational health.
By pinpointing improvement areas, analyzing revenue trends, and measuring against industry standards, providers gain critical insights for enhancing revenue and efficiency. Comprehensive reporting ensures regulatory compliance and financial transparency, enabling healthcare organizations to develop strategic plans for long-term growth and stability. AM Billing Care’s analytical approach delivers actionable financial intelligence to optimize revenue cycle performance.
Compliance and auditing form a critical component of revenue cycle management, requiring strict adherence to internal policies, legal regulations, and industry protocols. Regular audits enable healthcare organizations to verify their revenue cycle operations meet all standards while functioning effectively.
The audit process serves to identify potential risk areas and prevent billing errors or fraudulent activities. These measures help maintain both the financial integrity and ethical standards of the healthcare revenue cycle. AM Billing Care’s compliance-focused approach ensures revenue cycle processes meet all regulatory requirements while optimizing financial performance.
How Only AM Billing Care Offer Exceptional RCM Services?
AM Billing Care serves as your trusted revenue cycle management partner, helping maximize your revenue potential while handling all administrative tasks. Our certified professionals manage your billing operations with expertise, enabling you to focus entirely on delivering exceptional patient care.
With 24/7 support and proven results, we help healthcare providers achieve their financial and operational goals. Partner with us to enhance your practice’s growth and efficiency.

Ensure Billing Compliance

Improve Billing Process

Speeds Up the Revenue Cycle

Reduces Labor Costs & Billing Errors

Focus On Patient Care

Increases Practitioners Revenue

24/7 Support

Access to Expert Consulting
What Makes AM Billing Care Exceptional?
As a leading organization with a track record of exceptional achievements, AM Billing Care takes pride in consistently delivering timely and accurate results, boosting revenue, and helping clients achieve their financial goals. We use advanced expertise to streamline the Medical Billing process, improve productivity, reduce errors, and provide optimized customer service.
AM Billing Care has a team of highly experienced and skilled Medical Billing and Coding experts. Our expertise goes beyond managing billing requests—we also help you achieve your financial goals in the Revenue Cycle Management industry.
Why Do Healthcare Professionals Choose Our Medical Billing Services?
Our Revenue Improvement Services
Revenue Cycle Management is vital for healthcare organizations to ensure financial stability and maintain profitability. However, this task involves lots of complications, particularly when dealing with delayed payments, billing errors, and denied claims. That’s where you need AM Billing Care. Our time-proven and tailored revenue improvement services easily take you out of challenging situations and help your organization maximize cash flow while optimizing charges.

Comprehensive Assessment

Strategic Implementation

Credentialing & Contracting

Dedicated Staff Training

Increase Revenue

Customized Reporting

Continuous Education Training

Proactive Analysis

Medical Billing Software We Leverage for Revenue Cycle Management
Here are some Industry top listed EHR being operated by us.



















Frequently Asked Questions
Revenue Cycle Management (RCM) is a key financial process in healthcare that involves the managing of a patient’s financial transactions with a healthcare provider, from the initial point of contact through the final payment or resolution of any outstanding bills. It begins when a patient schedules an appointment and ends when the final payment for the appointment and treatment has been collected from responsible parties.
The primary goal of Revenue Cycle Management services is to improve and streamline the processes related to billing, claims processing, and payment collection to ensure that healthcare providers receive timely and accurate reimbursement for their services.
Key components of Revenue Cycle Management typically include.
- Patient Registration
- Charge Capture
- Insurance Eligibility Verification
- Claims Submission
- Claims Processing
- Payment Posting
- Denial Management
- Patient Billing
- Follow-up and Collections
- Reporting and Analysis
Revenue Cycle Management (RCM) offers several benefits to healthcare organizations, including hospitals, clinics, physician practices, and other healthcare providers. Some of the key advantages of effective RCM include.
- Improved Financial Performance
- Reduced administrative burden
- Increased reimbursement rates
- Enhanced Patient Satisfaction
- Compliance and Accuracy
- Faster Reimbursement
- Reduced denials
- Improved patient satisfaction
Improving Revenue Cycle Management (RCM) includes implementing strategies and best practices to restructure processes, enhance efficiency, reduce errors, and accelerate reimbursement.
Here are several steps you can take to improve your RCM:
- Staff Training and Education
- Improve your patient scheduling process
- Get pre-authorization for all necessary services
- Automate RCM Processes
- Verify Insurance Eligibility
- Accurate Documentation and Coding
- Insurance Contract Negotiation
- Prevent Claim Denials
- Streamline Billing and Collections
- Regularly Update Fee Schedules
- Use Clear Communication
- Monitor Key Performance Indicators (KPIs):
- Implement Revenue Cycle Analytics
- Compliance and Audit Controls
- Enhance Patient Registration
- Regularly Review and Update RCM Processes
- Implement best practices
The best practices for Revenue Cycle Management Services (RCM) vary depending on the size and needs of the healthcare organization. However, there are some general best practices that all RCM services should follow.
- Patient Education and Communication
- Insurance Verification
- Accurate Documentation and Coding
- Claim Submission and Management
Claim Denial Management - Automate RCM Processes
- Revenue Cycle Analytics
- Billing and Collections
- Contract Management
- Compliance and Audit Controls
- Staff Training and Development
- Regular Process Review and Improvement
Revenue cycle management (RCM) in healthcare faces several challenges, which can impact the financial health of healthcare organizations and create administrative burdens. Some of the common challenges include
- Complex and Evolving Regulations
- Reimbursement complexity
- Denial management
- Patient collections
- Technology challenges
Outsourcing Revenue Cycle Management (RCM) services can offer several advantages and disadvantages for healthcare organizations. It’s important to carefully consider these factors when deciding whether to outsource RCM.
Advantages of RCM Outsourcing.
- Improved cash flow
- Reduced administrative burden
- Increased reimbursement rates
- Reduced denials
- Improved patient satisfaction
- Access to expertise
Disadvantages of RCM Outsourcing.
- Loss of Control
- Confidentiality and Security Concerns
- Communication Challenges
- Risk of Mismanagement
- Initial Transition Challenges
- Long-Term Costs
- Potential for Overreliance
Revenue Cycle Management (RCM) for hospitals refers to the process of managing and optimizing the financial aspects of a healthcare facility’s operations to ensure accurate and timely collection of revenue for the services they provide. In simpler terms, it involves all the administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue.
Our team of experts can help you resolve denied claims, reduce billing errors, and post accurate payments. We can also help you optimize your charges, hold data entry professionals accountable, and provide customized solutions tailored to your specific needs.
How can AM Billing
Our team of highly skilled coders carefully review operative reports and encounter notes, check for over-coding and under-coding, and ensure that all billable procedures are accurate and proper.
Operational accountability involves holding experienced data entry professionals accountable and identifying areas for improvement. This service can help you eliminate issues involved in collecting bills on time.